On Friday night of the 2014 Labor Day weekend, I went to bed with my mortality in its usual full swagger mode, and I woke up on Saturday morning with my worldview entirely changed. Like most of us, we wake up bleary-eyed with cobwebs in the eyes and a mild bit of some unfocused vision. For some odd reason, the lower part of my vision in my right eye seemed to be more than the typical haze and cloudiness; it wasn’t there.
Optometrist
Even though it was a Saturday on a holiday weekend, we called my Optometrist’s office and got a hold of the on-call Doctor. We met the Doctor down at his office, and he ran a slew of tests, and he did determine that the vision in the bottom third of my right eye was gone. The problem now was trying to figure out what was going on. He got his textbooks and other office information out on the issue to focus on the diagnosis. Finally, he consulted with a Retina Specialist in town, who felt it was a BRAO or Branch Retinal Artery Occlusion. The Optometrist couldn’t do much more, so he made an appointment for me with the Retina Specialist for the following week.
Retina Specialist
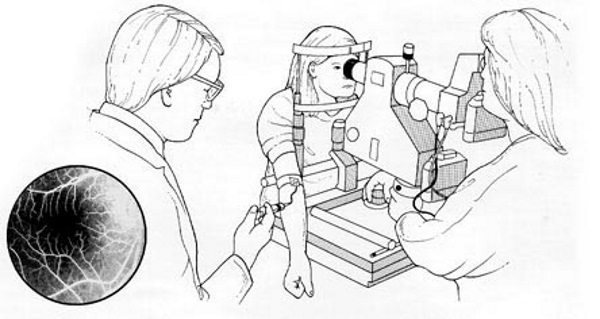
The Retina Specialist did some basic eye exams and needed a more in-depth analysis, so they did an Intravenous Fluorescein angiography (IVFA). It’s a technique for examining the retina’s circulation using a fluorescent dye and a specialized camera. It involves an injection of sodium fluorescein into the circulation, and then an angiogram is obtained by photographing the fluorescence emitted after illumination of the retina with a blue light.
He was adamant that I had an eye stroke between the various tests, which caused the BRAO. The central retinal artery, a branch of the ophthalmic artery, enters the eye through the optic disc and divides into multiple branches to perfuse the retina’s inner layers. A branch retinal artery occlusion (BRAO) occurs when one of these branches of the arterial supply to the retina becomes occluded (clogged).
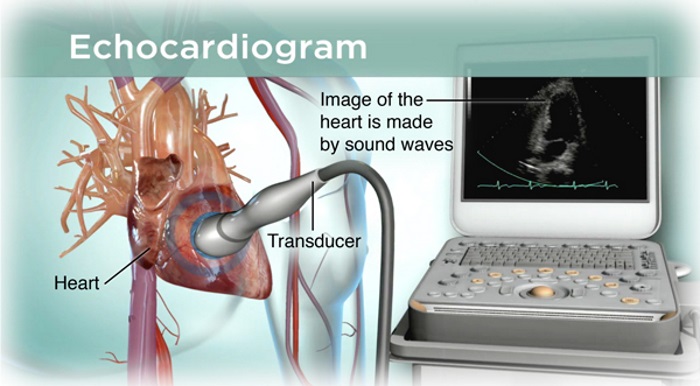
After the primary diagnosis was determined, we needed to determine why it happened, though he likely told me we’d never know the actual reasons. Did I have a heart issue, hypertension, elevated lipids, etc.? The Retina Specialist wrote up a lab to run some blood tests and an Echocardiogram and Carotid Ultrasound.
Cardiologist
At the same time, I made an appointment with a Cardiologist who ran an EKG and a Bubble Echocardiogram, and the latter looks for holes in your heart. He looked at the Echocardiogram (Standard and Bubble) and Carotid Ultrasound. Still, none of the tests showed anything out of the ordinary, though one blood test showed I had elevated lipids. It was interesting that my lipids were within the normal range, but now that I was an at-risk heart patient, they were considered elevated.
Neurologist
The next appointment I wanted to make was with a Neurologist, but they are tough to see and can take several months or longer to get in the door. Fortunately, my Wife knew someone that played the bassoon in the Denver Symphony that had connections to the Neurological Department at the University of Colorado Health Center. Almost overnight, I had an appointment up in Denver with a highly recommended Neurologist. She asked a bunch of questions about my history and genetics and then ran a slew of blood tests, covering just about anything that might be related to the heart, brain, genetic markers, and my diagnosis. Many gallons of blood later, only elevated lipids came up as an issue. She recommended staying on Asprin as an anti-platelet and perhaps adding a Satin, such as Lipitor, for the Cholesterol.
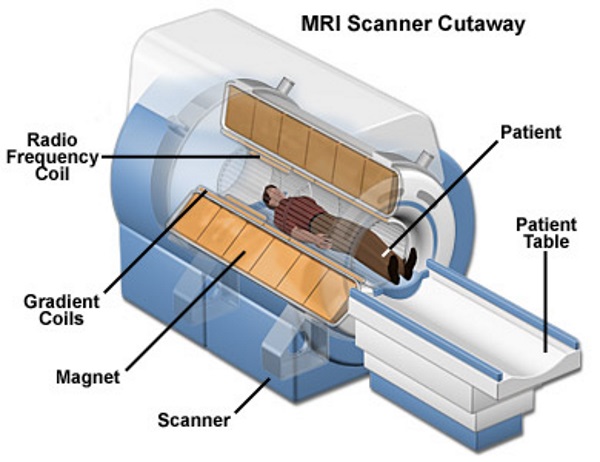
Since nothing outlandish came from the questioning and blood tests, she ordered three MRI sets for additional clues. They ran an MRI Brain w/o Contrast, an MRI Angiogram Head w/o Contrast, and an MRI Angiogram Neck w/o contrast and they took place in the wee hours of the morning and lasted for over an hour. Again, nothing conclusive came from the expensive and lengthy tests.
Diagnosis: Hyperlipidemia (abnormally elevated levels of any or all lipids) and BRAO
Neuro-Ophthalmologist
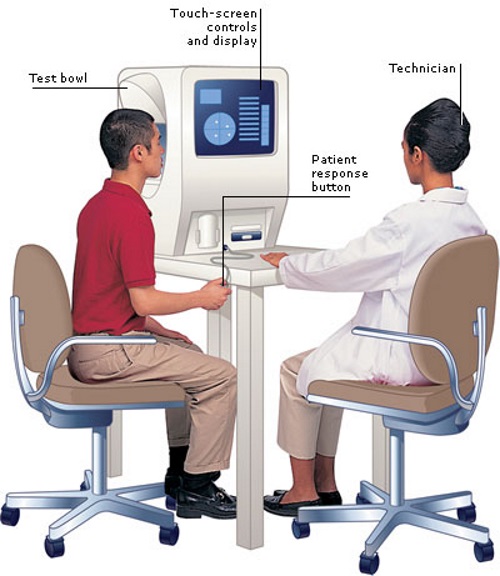
Next, I saw a Neuro-Ophthalmologist, which I never knew existed. She asked more questions, did some eye tests, and then performed a long-winded Visual Field Test. It’s an eye examination that can detect dysfunction in central and peripheral vision, which might be from various medical conditions such as glaucoma, stroke, pituitary disease, brain tumors, or other neurological deficits. Again, no conclusions of any sort.
Neurologist and Cardiac Telemetry
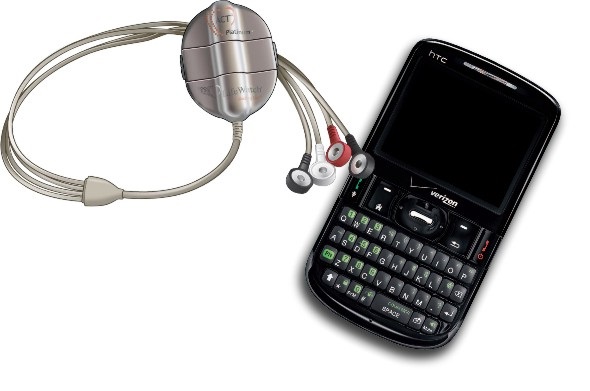
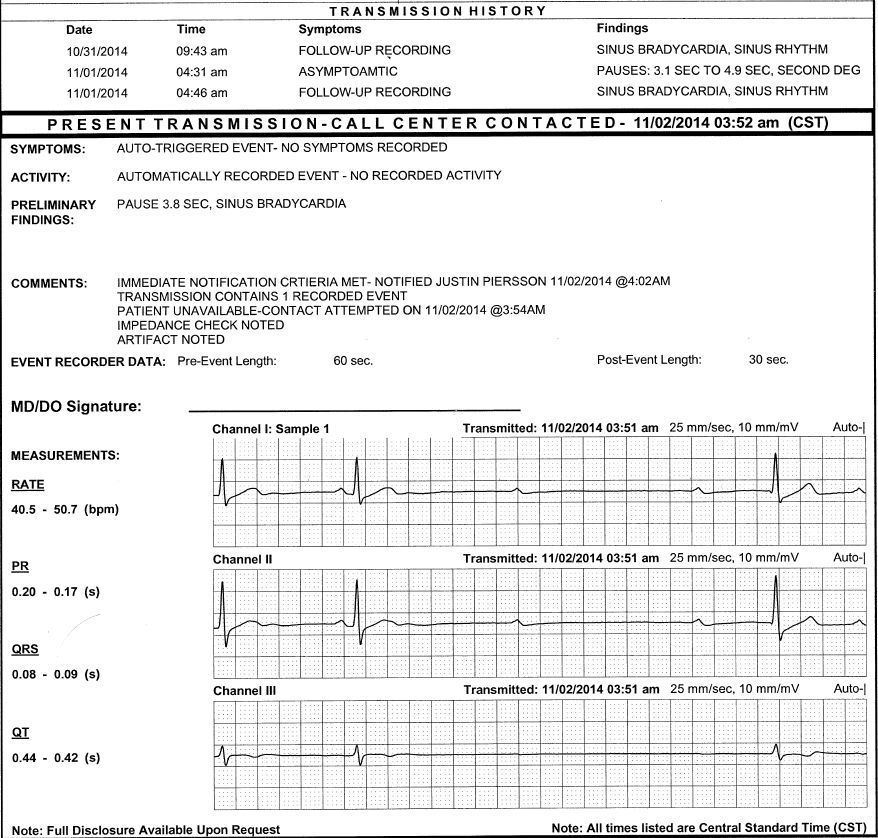
I asked my Neurologist if I could wear a heart monitor for a month per an earlier recommendation. I wore a LifeWatch Mobile Cardiac Telemetry Auto-detection system for the next 30 days. The system consists of a wireless sensor you hang from your neck and has four electrodes that you attach to specific locations on your chest. The electrodes pick up heart rate data and wirelessly sends its data to a companion cell phone, which in turn collects the information and pass it along to the LifeWatch monitoring center. It does auto-detection of AFib, Tachycardia, Bradycardia, and pauses information, along with daily summary and end of session reports with an AFib burden, heart rate histogram, and arrhythmia statistics. Not much happened most of the time, but at least a couple of times a week at 4-5 in the morning, the phone would ring, and a LifeWatch team member would ask if the wearer was having heart issues or shortness of breath? Of course, I was sound asleep and rarely even heard the phone calls, but it certainly woke up my Wife. Nothing seemed to be happening to me, and I never noticed anything going on when those calls would occur. Upset Wife!
When I spoke to the Neurologist, it turned out that my heart was taking 3-6 second pauses, which are known as a Ventricular standstill (VS). It’s a rare electrophysiological abnormality in which the heart stops beating and stands perfectly still. They also found Sinus bradycardia, which means the heart’s sinus rhythm is lower than average, usually in the ’40s, which isn’t a worrisome event.
Diagnosis: Mobitz (type) II Atrioventricular Block (electrical conduction block between the atria and ventricles) and BRAO
Cardiologist
Back to another cardiologist who performed a very detailed Echocardiogram (ECG) and asked tons of questions. He didn’t see anything outlandish in any previous test, the MRI’s or blood work, or the current ECG but was worried about the heart pauses, so he wanted to do a Stress Test before I went to see the Electrician. In Cardiologist parlance, the Electrician or Electrophysiologist works on heart rhythm disorders and the heart’s electric system. I did not want to see the Electrician since he might push me towards a Pacemaker, and that entire train of treatment sounds incredibly outlandish.
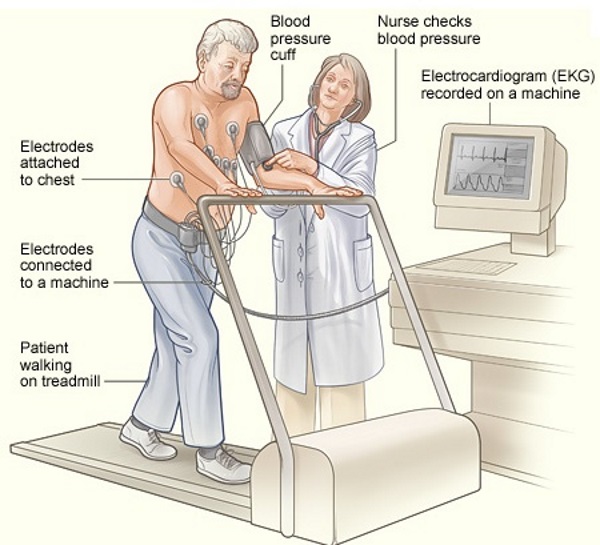
The Stress Test is an exercise Echocardiogram test performed on a treadmill that evaluates how your heart responds when pushed or stressed. First, they did an Echocardiogram while I was at rest, then I jumped on the treadmill with all the electrodes still attached and pushed myself until I was winded or at my max heart rate. The treadmill system is automatic and has seven levels of difficulty, and with each level, the treadmill gets faster, and the pitch steepens. I reached the end of level six (seven is the max) before I hit the wall and then had to jump over onto the gurney while the technician did another Echo; this one was while I was stressed. They’re also continually doing an Electrocardiography (ECG or EKG) during the entire test to check your heart’s electrical activity during the stressing procedure.
The conclusions from the Cardiologist were that I had the heart of a 25-year-old and did not have any heart-related issues and could skip seeing the Electrophysiologist. He said that they see the heart pauses during a deep sleep with many extreme and elite athletes.
Final diagnosis: Arrhythmia and BRAO
Retina Specialist
I went back one more time to see my Retina Specialist, who did some mild eye checks and told me that the eye stroke was a fluke. A random clot got pushed from somewhere in my bloodstream or heart and ended up in the artery of my right eye and occluded the bottom 35-40% of my vision. Glad the little clot didn’t end up in my brain.
Final Thoughts
Has my vision changed in the two years since it happened? My right eye vision’s bottom reaches are gone permanently, and I have had to make adjustments for that blind spot, though it still has 20/20 acuity. At least it didn’t obscure the central portion of my vision, which would have been life-altering. It hasn’t been a hindrance while bike riding and other sports, though I sometimes run into things since I can’t see them down by my feet, and frequently have to walk with my short Wife on my left side, so I don’t walk into her.
Am I worried about my heart? Yes, I am always concerned about it. I carefully pay attention to my heart rate while bike riding and always keep it within reasonable and safe zones. I accomplish this by wearing a heart rate monitor and viewing the status on a bike computer.
I no longer feel immortal, and I think about the shortness of life. The eye stroke has focused my attention on living in the now and all of the preciousness of friends, family, life, and the world’s beauty.








{ 0 comments… add one now }